LEARNING OBJECTIVES
JUMP TO LINKS:
The male reproductive system consists of:
- The testes where both production of spermatozoan and the sex hormone, testosterone, occur
- A duct system leading from each testis wherein spermatozoa are stored and undergo maturation
- Accessory sex glands that provide a fluid vehicle for the germ cells and whose peristaltic reflexive contractions contribute to the force required to eject semen
- The urethra which courses through the prostate and penis

Image: Gartner & Hiatt (2007). Color Textbook of Histology: Saunders Elsevier, p. 490
TESTIS
The testes develop in the abdomen and descend into scrotum during fetal development. Testes are maintained slightly below body temperature, an important condition for sperm production.
Each testis is covered with a thick capsule, the tunica albuginea which, in turn, is covered on its anterior and lateral margins by the tunica vaginalis, derived from the abdominal peritoneum. The posterior border of each testis capsule is greatly thickened and extends into the substance of the gland to form an incomplete partition, the mediastinum testis. Fibrous septa extend from the mediastinum to form approximately 250 pyramidal compartments, the testicular lobules. Each lobule is occupied by 1-4 seminiferous tubules surrounded by loose connective tissue rich in blood and lymphatic vessels, and nerves. The seminiferous tubules produce spermatozoa and the interstitium contains the second major component of the testis, the interstitial or Leydig cells which produce testosterone.

Image: Gartner & Hiatt (2007). Color Textbook of Histology: Saunders Elsevier, p. 490
SPERMATOGENESIS vs. SPERMIOGENESIS
SPERMATOGENESIS
Spermatogenesis refers to the entire process by which spermatogonia (stem cells) give rise to spermatozoa.
The seminiferous tubules consist of a tunic of fibrous connective tissue, a well-defined basal lamina, and a complex seminiferous epithelium. The tunica propria contains several layers of fibroblasts and myoid cells that probably assist in expelling spermatozoa from the tubules.
The seminiferous epithelium consists of cells of the spermatogenic lineage, stacked in 4-8 layers, and supporting Sertoli cells. The cells in the spermatogenic series represent various stages in the continuous process of differentiation which leads to the formation of spermatozoa. This process can be divided into 3 phases:
- Spermatocytogenesis: Division of spermatogonia which give rise to spermatocytes. Spermatogonial types include Type A and Type B spermatogonia.Type A spermatogonia consist of two types. Dark Type A spermatogonia act as a reserve population. Pale type A spermatogonia undergo mitosis to become Type B spermatogonia. Type B spermatogonia give rise to spermatocytes. All daughter cells remain connected by cytoplasmic bridges, forming a syncytium as meiosis progresses.
- Meiosis: Spermatocytes undergo two meiotic divisions to produce spermatids.
- Primary spermatocytes undergo meiosis I
- Secondary spermatocytes undergo meiosis II
SPERMIOGENESIS
Spermiogenesis refers to the process by which spermatids undergo elaborate cyto-differentiation to produce spermatozoa, including shedding their cytoplasm and gaining a tail, known as the flagellum.
Image: Gartner & Hiatt (2007). Color Textbook of Histology: Saunders Elsevier, p. 497
–Proacrosomal granules coalesce within a portion of Golgi into a single acrosomal granule contained within a vesicle. Granule and membrane spread over the anterior half of the condensing and elongating nucleus. Now called the acrosome this structure serves as a special kind of lysosome containing hydrolytic enzymes that include hyaluronidase, hydrolases and proteases which will assist in penetrating the granulosa cells and the zona pellucida surrounding the egg.
– Simultaneous with acrosome development the centrioles migrate to the opposite pole of the nucleus and form the flagellum. Flagellar movement is powered by mitochondria that are aligned in a spiral array around the proximal flagellum.
– As differentiation proceeds most of the surplus cytoplasm is cast off, leaving a thin cytoplasmic covering for the sperm head, mid-piece and tail.
– Development from spermatogonia to the spermatid stage takes 74 days. Sperm subsequently acquire the potential to become motile in epididymis and undergo further maturation (capacitation) in the female genital tract.
– Fertility: The normal ejaculate consists of 3 ml of semen with 100 million sperm/ml. Less than 20 million sperm/ml is associated with sterility. Fertility may be retained when up to 20% of the sperm are abnormal. Abnormalities can result from ionizing radiation, heat, certain drugs, carcinogens and mutagens.
Sertoli cells
Sertoli cells are large pyramidal cells that envelope the cells of spermatogenic lineage. Tight junctions between these cells form the blood testis-barrier and divide the seminiferous tubules into basal and adluminal compartments.
The spermatogonia in the basal compartment are directly exposed to blood-borne materials in the interstitial fluid. In contrast, materials must reach the spermatogenic cells in the adluminal compartment via the Sertoli cell cytoplasm.
Sertoli cell function includes:
(i) producing testicular fluid
(ii) concentrating testosterone
(iii) translocating interconnected germ cell progenitors to the lumen and actively release mature sperm to the lumen
(iv) disposing of residual bodies
(v) secreting müllerian inhibiting substance (anti-müllerian hormone) during embryological development

Image: Gartner & Hiatt (2007). Color Textbook of Histology: Saunders Elsevier, p. 492
Functional significance of the blood-testis barrier:
(i) Maintains optimal environment (nutrients, hormones) for sperm cell differentiation
(ii) Isolates and protects differentiating sperm from damaging substances in the blood
(iii) Prevents sperm antigens from reaching the rest of the body (preventing possible autoimmune responses to developing sperm at puberty).
ENDOCRINE FUNCTIONS
Leydig cells
Leydig cells are located in the interstitium between the seminiferous tubules and produce the steroid sex hormone testosterone.
Testosterone functions in spermatogenesis; in the development and secretory activity of accessory sex glands; and in the development of male secondary sexual characteristics.
(i) Spermatogenesis: Regulation of androgen secretion and function depends on the gonadotropic hormones FSH and LH produced by the anterior pituitary. These agents are, in turn, under the regulation of FSH and LH releasing hormones from the hypothalamus.
LH stimulates Leydig cells to produce testosterone. FSH stimulates Sertoli cells to synthesize androgen binding protein (APB). Testosterone taken up by Sertoli cells binds to APB and the complex is secreted into seminiferous tubule lumen where it acts to stimulate spermatogenesis.
Negative feedback loops: Elevated testosterone levels act as a negative feedback stimulus to inhibit FSH/LH-RH. Sertoli cells also produce inhibin which inhibits release of FSH.
(ii) Male secondary sexual characteristics: Testosterone also influences development of secondary sex characteristics, libido, proper maintenance of genital glands and ducts, and aggressiveness.

Image: Gartner & Hiatt (2007). Color Textbook of Histology: Saunders Elsevier, p. 501
GENITAL DUCT SYSTEM
Intratesticular Ducts
(i) Straight tubules (Tubule Recti): channels continuous with seminiferous tubules and rete testis. They are lined by Sertoli cells only.
(ii) Rete testis: Channels in the mediastinum lined by simple cuboidal epithelium.
(iii) Efferent ductules: epithelial lining consisting of alternating groups of columnar cells with cilia and cuboidal cells (scalloped appearance). Ciliary movements propel sperm to the epididymis; cuboidal cells absorb fluid produced by the seminiferous tubules.
Extratesticular Ducts
Epididymis:
Lined by pseudostratified epithelium with stereocilia. The epididymis is a site of sperm maturation (acquisition of potential for movement) and storage. Together with the efferent ductules the epididymis absorbs 90% of the seminiferous fluid. Circular muscle layers propel sperm by peristaltic contractions.
Ductus Deferens:
Lined by pseudostratified columnar epithelium with stereocilia. Contraction of the muscular wall (longitudinal inner and outer layers, circular middle layer) propels sperm towards the ejaculatory ducts & urethra.
Accessory Sex Glands
Seminal Vesicles:
Approximately 15 cm long tube that is coiled and convoluted on itself. Extremely folded mucosa with pseudostratified columnar epithelium. Lamina propria is surrounded by layers of an inner circular and outer longitudinal muscle layer. Seminal vesicles synthesize sperm activating substances including fructose (a forensic marker), citrate, inositol, prostaglandins and proteins.
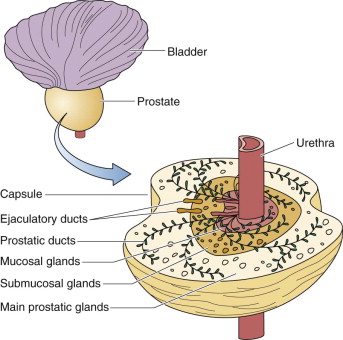
Prostate:
Aggregate of 30-50 small compound tubulo-alveolar glands that drain via approximately 20 ducts into the urethra. The secretion is rich in proteolytic enzymes which aid in liquefaction of the semen. Also contains large amounts of acid phosphatase which is elevated in cases of prostatic carcinoma (diagnostic).
Glands are grouped into mucosal glands, located around the lateral and anterior portion of the urethra, and submucosal and main glands in the rest of the prostate. Hyperplasia of the mucosal glands is common in men over 50 and can cause urethral obstruction. Carcinoma of the prostate is the second most common form of cancer in males. Clinical correlates: Benign prostatic hyperplasia & prostatic adenocarcinoma
PENIS
Consists of 3 cylinders of erectile tissue:
- 2 Corpora cavernosa dorsally
- 1 Corpus spongiosum ventrally – contains penile urethra.
The corpora consist of networks of irregular vascular spaces lined by endothelium and separated from one another by partitions (trabeculae) composed of dense fibroelastic tissue with smooth muscle bundles. Each cylinder is surrounded by a thick fibrous sheath, the tunica albuginea. The surrounding connective tissue, which contains many smooth muscle fibers, is covered by skin.
 Image: Gartner & Hiatt (2007). Color Textbook of Histology: Saunders Elsevier, p. 507
Image: Gartner & Hiatt (2007). Color Textbook of Histology: Saunders Elsevier, p. 507
Erection Mechanism: Erection is brought about by parasympathetic induced relaxation of the arteries supplying the vascular spaces of the penis. Vascular dilatation causes blood to enter and distend the corpora and the resultant compression of the draining veins leads to engorgement and erection of the penis. After emission, which is an autonomic sympathetic response, the arterial walls regain their former tonus.
Images: Gartner & Hiatt (2007). Color Textbook of Histology: Saunders Elsevier, pp 489-510
